Have Standard Low Back Treatments FaIled You?
Do you suffer from ongoing back problems or sciatica which mean you are struggling to reclaim your life?
Maybe you’ve tried some of these treatment options:
- your usual physio, chiropractor or osteopath
- hands-on therapies: adjustment, mobilisation or massage
- hands-off therapies: exercise, Pilates or dry needling
- different medications
- injections
- rhyzolysis
- surgery
Perhaps you’ve even made an impulse purchase that promised the world but delivered little.
You’ve probably tried all the ‘miracle’ exercises and stretches on YouTube too.
You might feel like you are on an endless treadmill from investigation to medication, specialist, therapist and back to the start again.
So what’s next? What do you do when the ‘usual’ therapies fail?
It can be hard to see a way out, but there is hope!
Recent Australian research is pointing towards different, innovative back pain treatments that challenge the ‘standard’ back pain physiotherapy treatment.
This article will give you a taste for these modern ideas by presenting the current best practices for low back pain relief.
I’ll also share some resources that we use in the clinic that you can access.
Here is a summary of the steps:
Quick Summary
How To Help Your Persistent Low Back Pain
Click on each step to learn more
Rule out ‘red flag’ conditions: this may have been done by your GP or physio but it’s an important step not to miss
Assess if the back pain acts mechanically: even when pain has been present for months and years, there can still be a mechanical element to address
Learn about your pain: finding out that your back pain isn’t just about your back can be challenging but ultimately can be the game-changer
Innovative brain exercises: help improve the ‘map’ in your brain, the way that your brain ‘sees’ your back
Pace yourself: have a plan of physical activity (and even social activity) that uses the principles of graded exposure to ‘get under the radar’ of the pain system
Exercise: cover the three areas – general exercise, strengthening exercise and movement
Reduce systemic inflammation: there are steps you can take involving regular exercise, good sleep habits and a health diet to help you hurt less
Get a fresh perspective: if you are stuck in a rut, it might be good to get a fresh set of eyes on the problem if things are not changing or getting worse.
Rule out 'red flag' conditions
Before you go any further, have you had ‘red flags’ ruled out?
‘Red flags’ are clues from either your description or the physical examination that could indicate something serious or sinister.
These things are usually rare, but they do happen.
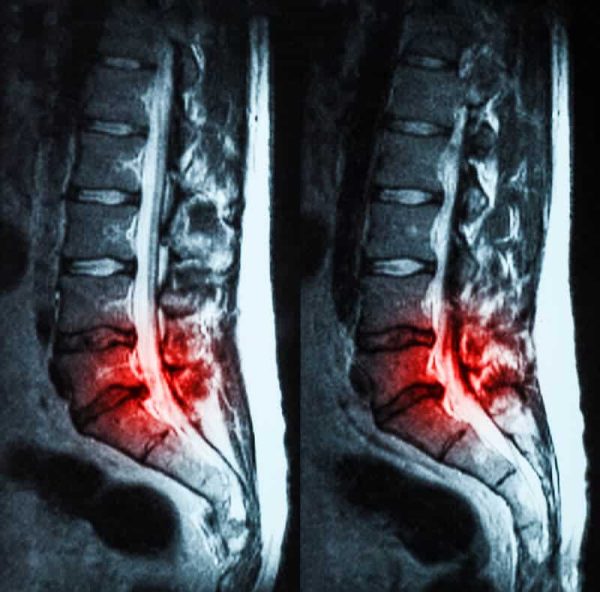
If your GP is suspicious about your signs or symptoms, they will send you for an investigation like an MRI or a CT, and perhaps blood tests.
It is widely recognised that these investigations are overused for low back pain and often not needed. However, one situation where imaging is definitely worthwhile is investigating suspected red flags.
Since most back pain presentations don’t need imaging, don’t be disappointed if your GP doesn’t send you for an MRI. It is not best practice to get imaging for everyone with lower back pain.
They have been shown to be more harmful than helpful when they aren’t required.
If your physio has any concerns about one of these conditions, they will typically suggest that you visit your GP for their opinion or further investigations.
You can read more about cauda equina syndrome, which is one important red flag condition that we screen for.
Once you have had red flags ruled out, the next step is really important …
Assess if the back pain acts mechanically
Regardless of the duration of the back pain episode, a systematic assessment process is needed to establish if there is a mechanical cause for back pain.
A mechanical cause simply means a cause that is related to a low back structure that is going to respond to some kind of direct treatment.
A system like the McKenzie Method can help quickly and accurately determine if this is a back pain that can be changed rapidly.
The McKenzie assessment works to categorise a problem into one of four categories. The first category is when a directional preference is found, meaning a direction of movement that rapidly changes things and remains that way ie it’s not just the first moment when you hop off the bed, but for example you can bend better with less pain and it remains.
If a directional preference is found, this needs to be explored and treated thoroughly, but it doesn’t detract from the next very important element …
Learn about your pain
One of the most important elements of successful physiotherapy treatment of persistent back pain is to learn more about your pain and how it works.
This might seem like a weird way of treating back pain!
However the research shows that this can be absolutely pivotal in helping persistent pain problems. We have found that to be the case in our experience as well.
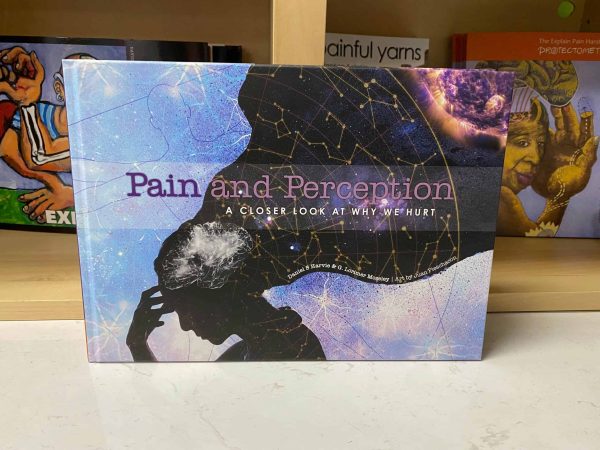
Books we use and recommend
Explain Pain – David Butler and Lorimer Moseley
Protectometer: The Explain Pain Handbook – David Butler and Lorimer Moseley
Painful Yarns – Lorimer Moseley
Pain and Perception: A Closer Look At Why We Hurt – Dan Harvie and Lorimer Moseley
Why Does It Still Hurt – Paul Beigler
We have other blogs on the topic of helping to understand pain.
This is a collection of short pain science nuggets of information that are digestible and easy to understand,
Why is learning about pain science helpful if you have persistent back pain?
You might think ‘I know all about my pain – I live with it every day’.
That is true, but we also know that learning about the biology of how pain works allows you to look at your experiences through a new lens.
This in itself can be very liberating.
Two of the key concepts are these:
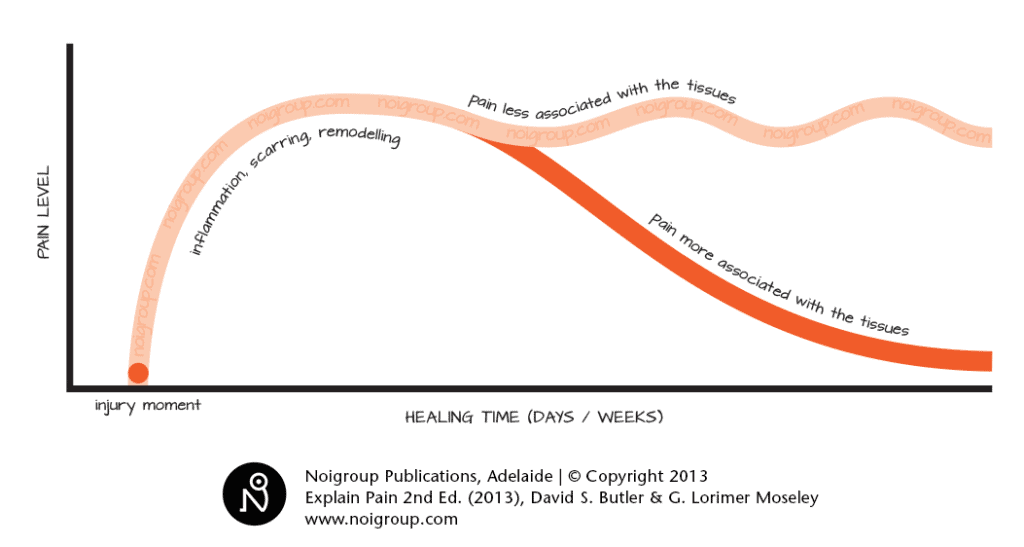
- Pain and injury are not the same thing – you can have one without the other.
- The longer you experience back pain, the less reliable and the less accurate the information it provides about your back.
Therefore, the pain becomes less ‘helpful’.
It starts to behave under the theme that it is ‘better safe than sorry’.
It is like your body errs on the side of caution.
As a result, your pain can continue long after an injury is fully healed.
Understanding some pain neuroscience will help you to know:
- When you should pay attention to your pain
- When it is OK to have pain and how much is OK
- When resting won’t help
- When you can safely do more
- How to reduce your pain through movement and activity
In short, it will help to give you the confidence to move.
This can be a game changer!
Patients get the best results when they read about it, or watch a good explainer video, and talk it through with an informed health professional.
Most people hit some learning snags along the way, when something doesn’t quite make sense. Dealing with these snags when they happen makes it easier to keep learning.
A good back pain physio with the right knowledge and experience can make all the difference.
It is impossible to overstate how important this step is.
A working knowledge of pain science powers everything to come …
Understand why you hurt and you will hurt less
David Butler
Free Online Pain Course
This course is 6 weeks long and it is sent straight to your inbox each week. Each week’s email contains a link to the learning module.
This is information is a mixture of reading, video clips and other resources to make the learning easy and entertaining.
You do have to devote a little time to this (maybe 20 minutes per week), but if you want to learn something new, there is no alternative!
The benefit is that this new knowledge will give you confidence and freedom, not to mention hope that there are other approaches that work apart from a pharmaceutical approach.
Innovative brain exercises for back pain
If you don’t understand how pain works, the idea of doing brain exercises to help your back pain might seem weird.
However, it makes more sense if you understand these two ideas:
- neuroplasticity – the way continues to learn and change all through life
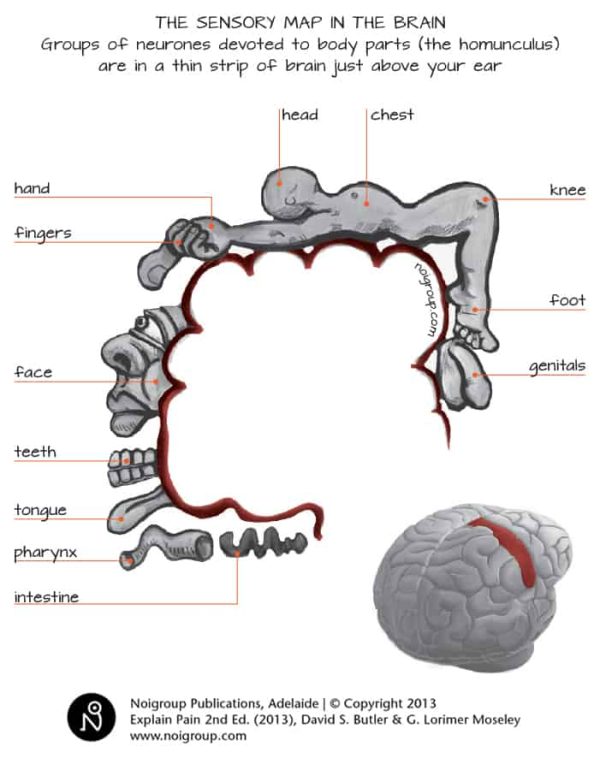
- your brain has a ‘representation’ or a ‘map’ of your back region that subtly changes with persisting pain
Researchers have shown that the ‘map’ of the back region gets less precise and more easily triggered as pain persists.
This also helps to explain the way that back pain can spread.
For a long time we have suspected that addressing this was important, but the RESOLVE trial (see below) now gives even stronger evidence to do so.
Apps we use and recommend
- Protectometer app
- Recognise app
These are available on the usual app platforms and designed for mobile devices rather than desktop.
What evidence is there that brain exercises are best practice?
On their own, brain exercises aren’t going to be a panacea.
They appear to be an important step on the path to improving how your brain ‘sees’ your back and reducing your back pain.
They work best alongside understanding your pain, and then actually using your back in a new way.
A landmark study called the RESOLVE trial was published in 2022 which studied the best form of back pain physio. It used pain education, brain exercises and innovative movement exercises and strengthening to treat chronic back pain.
The aim was to use this approach to reverse the brain changes that happen when you have back pain for a long time, and ultimately to reduce the participants’ back pain.
In the study, these brain exercises followed a progression from a small volume to a larger volume, from less ‘brain challenging’ to more ‘brain challenging’.
This is a concept known as graded exposure which is useful for persistent pain and many other conditions.
This next section contains another important way of applying graded exposure …
Pace yourself
The idea of pacing might not seem that innovative but it is often a key concept in getting ahead with low back pain.
The problem is … most of us are awful at it!
When things are going OK in our body, our lumbar spine and our protection system has a certain tolerance to doing a bit extra.
For example, you might be able to get stuck into the garden on the weekend and end up with a few sore back muscles (and others) for a few days, but that’s all.
However, with a hypersensitive protection system, back pain is easily triggered with small changes in activity, even when it really isn’t warranted.
Common pacing mistakes
People with ongoing back pain often have one of two approaches. Do you relate to either of these?
The ‘Let Pain Be Your Guide’ Approach: This is backing off when it hurts because the pain is telling them that is the right thing to do. More resting, less moving.
The problem: Progressively doing less and less, and reinforcing the hypersensitivity of the protection system. This makes it even easier to trigger your low back pain.
The ‘Boom-Bust’ Approach: This is maximising activity on days when things feel good, which then flares the back pain up good and proper. This flare-up of pain can lay you flat for days.
The problem: ‘Boom-busting’ also has the end result of turning up the protection system sensitivity as there is a further link between activity and more pain.

The secret to pacing
The secret is doing an amount of an activity that is not too extreme in either direction, and gradually increasing it over time. This is known as pacing, a kind of graded exposure to an activity.
Sounds easy, right?
However it can be anything but easy, and especially if you do it on your own.
We find that people often need quite a bit of help to find their baseline (the right starting point), and they need coaching to help stay on track and not pull the pin at the first sign of an increase in pain.
Once again, a solid understanding of pain is vital.
If you know that pain isn’t the result of harm but instead it is a result of your extra sensitive alarm system being triggered, it makes all the difference.
People who understand this can still freak out if their alarm system is triggered (it hurts after all!) so someone to guide and coach you is important.
Exercise for Low back pain
We know that there are lots of benefits of strengthening and cardiovascular exercise. It helps muscles, bone density, heart health, mental health and much more.
But did you know that exercise can also have a positive impact on pain?
What types of exercise help back pain?
Exercise that helps back pain can be broadly divided into 3 types:
- General exercise
- Strengthening
- Movement
General exercise is the kind of exercise that gets your heart rate up. This includes things like walking, swimming and cycling.
Which type is the best for you?
The answer is easy – the one that you are going to do and look forward to doing!
Strengthening for back pain makes most people think automatically of ‘core strengthening’.
If all you are doing is ‘core exercises’, you are missing out. I’m also talking about strength that involves your upper body and lower body too.
Correctly employed and at the right time, you can use lifting exercises as a way of allowing your alarm system to ease up.
Movement is an important aspect of exercise for helping back pain.
We know that all joints, muscles and nerves are designed to move and require movement to stay healthy.
Sometimes range of motion is important, sometimes it isn’t as important.
Movement is always important though.
Movement can be used for graded exposure and changing the sensitivity setting on the alarm system.
Movement with knowledge about the pain system is the most effective.

Virtual Reality - a truly innovative technique for back pain relief
Virtual Reality presents some amazing opportunities for helping persistent pain, including back pain.
The Virtual Reality platform that Reality Health have developed is based on the concepts of the RESOLVE trial, with the ideas presented in a novel way.
We have started using Virtual Reality in the clinic for back pain, and it covers each of these steps:
- pain neuroscience education, making it fun, interesting and more visual
- brain exercises by presenting movement in a different way to the brain and central nervous system
- movement coupled with brain exercises allowing people to move without fear in an enjoyable way
The potential benefits for using Virtual Reality with persistent low back pain and other types of persisting pain is huge.
Reduce systemic inflammation
- Adopting a healthy active lifestyle with regular exercise
- Establishing good sleep patterns
- Eating a healthy diet with a focus on more fresh and less processed foods.

Get a fresh perspective
Lastly, if you’re stuck in a rut with your back pain, it might be time to get a fresh set of eyes on your problem.
Getting a second opinion can be extremely helpful if it feels like things are going nowhere or getting worse.
Sometimes we find that is helps people to understand that they ARE doing the right things, and that they need to keep up the good work and persist.
Other times, we find that it helps to show people a viable alternative path like the one we have discussed.
But how do you know who you should be talking to?
We have written an article on 10 essential tips for choosing the right physio for you which has all the information you’ll need to make the best decision.
One of the best ways of finding out if they are right for you is speaking directly with the physio so that you can discuss your situation, and what solutions they offer.

Read more about our back pain physiotherapy service
If you have had other treatments that haven’t worked, you may be sceptical about seeing yet another practitioner with another set of promises.
Click to read this page about what can we offer you and how we go about it.
Hopefully you’ll see that we are not your average physio service!
Summary
The aim of this article was to show anyone with persistent low back pain that there ARE other approaches. And there is always reason for hope!
Each of the ideas that we have presented are science-based, up-to-date and best practice.
For example, the RESOLVE trial has provided evidence for the use of a combination of modern pain science education, graded motor imagery (brain exercises with pacing) with paced movement and exercise intertwined.
So what is the next step?
If you are:
- in trouble with persistent low back pain
- have tried all the ‘usual’ stuff without results
- ready to try something new and to take on the challenge
… here is how I would suggest approaching it.
- Make sure that any red flags are excluded. If you’re not sure that this has happened, speak with your physio or GP.
- Get a working knowledge of pain science using the resources in this article.
Signing up for our Free Online Pain Course would be a great idea! - Read of the article on the anti-inflammatory Diet and make some positive changes to your diet.
- Start engaging in some regular general exercise using the pacing principles.
- Find a modern, pain-science informed physio to be your companion, coach and mentor.
We offer an opportunity for anyone in the Adelaide region to speak directly with one of our physios to make it easy to gauge if we would be a good fit.
This is something that we offer freely because it allows our prospective patients to know if we are on the same page.
It also gives us a change to discuss some of the things we stand for and how we are a little bit different.
Would you like to speak with one of our back pain physios FREE OF CHARGE?
What’s holding you back? Let’s talk about it!
BOOK ONLINE or call us on (08) 7282 0871 and let’s lock in a time!
NB: This offer is for Adelaide residents only.
Frequently-Asked Questions
Here are some questions that we commonly get asked about back pain.
I also have pain in my buttock or running down my leg from my back. What does that mean?
That can happen for a few reasons. Referred pain from the back to the buttock and the thigh are common, with the brain ‘misunderstanding’ where the danger message is being generated from.
Leg pain can be related to related to nerve tissue being irritated and can have other symptoms like altered feeling.
If this is accompanied by weakness in some leg muscles and a loss of tendon reflexes, it is a sign of possible nerve root compromise.
Your back pain physio can give you a better idea of the cause of your leg pain.
Should I get a scan for my lower back pain?
While it might seem instinctive to get a scan, it is only recommended to check for ‘red flag’ conditions, or if the results would change the management plan eg surgery vs not surgery.
There is evidence to say that scans and other investigations can be more harmful than helpful if they aren’t required.
Scans will show you every little thing in your back. The problem is that the correlation between changes on the scans and pain are low.
What is causing my lower back pain?
There is never one cause, or one structure to blame – there are many factors that can involved.
There might be ’tissue’ factors like disc, muscle, nerve and more.
There might be non-tissue factors too, like your memory of a past incident, what you believe about your back, your immune system.
Traditionally, back pain has always been looked at in terms of a single tissue cause (a pathoanatomical approach), but we know that it is much more complicated than that and the longer it lasts, the less likely there is to be a single cause.
The truest statement is to say that your central nervous system (brain and spinal cord) has concluded that right now, there is something that needs protecting, and has switched on your pain protection system to give you the experience of pain in your lower back.