Cauda equina syndrome is a rare but very serious red flag condition associated with low back pain. In this blog, Lisa Vernon explains exactly what it is and why physios are asking about your bladder and bowel when you come in with a bad back!
What is the cauda equina?
You might be surprised to know that your spinal cord doesn’t end at the bottom of your back.
The spinal cord ends in the upper portion of the lumbar spine at about the level of L2. This can vary between T12 and L3 due to our normal anatomical variation.
The collection of spinal nerves that continue down the spinal canal from this point are collectively known as the cauda equina. It is made up of L2-5 nerve roots, all the sacral nerve roots S1-4 and the coccygeal nerve.
These nerves send and receive messages to and from the legs, feet and pelvic organs, including your bladder and bowel.
Why is it called the 'cauda equina'?
This is due to the cauda equina’s resemblance of a horse’s tail.
‘Cauda equina’ is Latin for ‘tail of horse’.

What is Cauda Equina Syndrome?
- Lumbar spinal stenosis
- Spinal infections and tumours
- Postoperative lumbar spine surgery complications
- Trauma to the lower back eg from gunshots, falls or motor vehicle accident
- Spinal anaesthesia
There are exciting developments in relief from back pain.
Learn more about the current best practice.
Is Cauda Equina Syndrome dangerous?
How common is it?
It is a relatively rare condition, but it is certainly possible for a GP or a physio to see a patient with cauda equina syndrome in their career. It is certainly something that every responsible health practitioner should screen for with a new patient with low back pain.
To give it some context, Cauda Equina Syndrome has been estimated to occur in 3% of disc herniations.
It is estimated that the annual incidence is 1.5 to 3.4 per million people, meaning that each year in Adelaide, there are 2.25 to 5.1 people diagnosed with this (Foresoefel & Moore 2002)
Why is it called a red flag condition?
Cauda Equina Syndrome is labelled a ‘red flag’ condition.
Red flags are conditions with a serious pathology that require further medical examination.
There are signs and symptoms found in the patient history and clinical examination that suggest there may be a situation that needs further investigation.
As first contact practitioners, physiotherapists are trained to screen for “red flags”, and it is a routine part of our examination.
How is Cauda Equina Syndrome diagnosed?
Below are the most common symptoms for cauda equina syndrome:
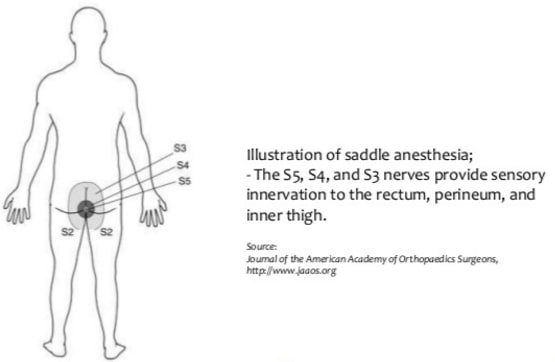
- Urinary retention – where an individual feels they have a full bladder but aren’t able to initiate urination
- Urinary and/or faecal incontinence
- Saddle area numbness or saddle paraesthesia – tingling, partial or full numbness of the area that you sit on a saddle. This might be first noticed when wiping with toilet paper feels different or numb
- of one or more muscles in the legs – this will depend on which nerve roots are affected
- Referred, sciatica-like pain in the legs
- Unexplained sexual dysfunction
- MRI: this produces images of the spinal cord, nerve roots and surrounding areas.
- CT scan: which gives definition of the bone. This is helpful if CES is secondary to bone collapse from trauma or cancer.
- Myleogram: An X-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces; can show displacement on the spinal cord or spinal nerves due to herniated discs, bone spurs, tumours etc
It is easy to see how a slow onset of these symptoms could easily mimic other conditions, delay diagnosis and lead to inappropriate treatment like manual therapy or medications for a urinary condition.
How do we help if the 'usual' treatments don't help?
If you have had other treatments that haven’t worked, I imagine you’ll be sceptical about seeing yet another practitioner.
We have a step-by-step plan of how we help people with back pain which hasn’t resolved, which you can read by clicking the button below.
What is the treatment?
Prompt diagnosis and treatment is the best treatment for patients with CES.
Emergency spinal decompression surgery is usually required to decompress the nerve roots of the cauda equina.
Treating patients within 48 hours after the onset of the syndrome provides a significant advantage to recovery of movement and feeling in affected areas and urinary and rectal function.
Take Home Messages
Cauda equina syndrome is a rare disorder, but that doesn’t mean it doesn’t happen.
When it does, it is serious.
All healthcare professionals need to be aware of the signs and symptoms and the importance of early diagnosis and intervention.
The treatment is usually a surgical emergency.
Early assessment and management leads to the best outcomes on restoring sensory and motor deficits.
Anyone who is experiencing alteration of their bowel or bladder function, sexual function or leg strength that is associated with an episode back pain or leg pain should see their GP or physio and discuss these symptoms without delay.
If there is reasonable suspicion, they should be evaluated by a spine surgeon as soon as possible.
References
Stuart, A., Cauda equina syndrome: Symptoms, treatment, surgery, and more. WebMD. Available at: https://www.webmd.com/back-pain/guide/cauda-equina-syndrome-overview [Accessed September 17, 2022].
Cauda equina syndrome. AANS. Available at: https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome [Accessed September 17, 2022].
Foresthoefel, C & Moore, D (2021) Cauda Equina Syndrome. Available at: https://www.orthobullets.com/spine/2065/cauda-equina-syndrome [Accessed September 17,2022]
Read more about our back pain service
If you have had other treatments that haven’t worked, you may be sceptical about seeing yet another practitioner with another set of promises.
Click to read this page about what can we offer you and how we go about it.
Hopefully you’ll see that we are not your average physio service!