Tendinopathy and tendon pain is something that can frustrate people of all ages and activity levels.
Tendinopathies are common and often quite persistent, and affect the ability to participate in sport, exercise, work and other leisure activities.
If you are looking to manage your own tendon pain, there is a lot of generic and misleading information on the internet about what is the best thing to do.
To help, physiotherapist Lachlan Sutherland has written this comprehensive guide to tendinopathy, why they get painful and the different treatment options.
He also discusses some of the persistent myths that you’ll read on some high profile medical websites.
An introduction to tendons
Tendons are an essential part of our musculoskeletal system.
They connect our muscles to our bones and allow us to create movement at our joints. Without them, we wouldn’t move!
(Compare this to ligaments which connect bone to bone and are designed to limit certain movements of the joint.)
Painful tendons are a very common sports injury, but they also happen in everyday life to non-sportspeople too.
This article is essential reading if you:
- have tendon pain and you’re not sure if you are being given good advice
- are confused with the different terminology about tendon problems
- have ‘tendonitis’ that has been slow to improve
- are concerned after having ultrasound imaging on your tendon
- have questions about if you are doing the right thing to help
In this article, we will discuss:
- What is a tendon?
- What happens in tendinopathy?
- The common causes of ‘tendonitis’
- How to tell if you have ‘tendinitis’
- The different locations of ‘tendonitis’
- Physio treatment for ‘tendinitis’
- Other treatments for ‘tendonitis’
- Why it’s difficult to fully recover from tendon injuries
- Tips for avoiding injuries and keeping tendons healthy and strong
- Common questions about tendons and tendinopathy
You might be wondering why ‘tendonitis’ and ‘tendinitis’ are in quotes, and why I have used both spellings.
This terminology is a good place to start to help clear up any misunderstandings.
Is tendinitis the same as tendonitis?
Yes it is, and strictly speaking the correct spelling is tendinitis.
This literally means ‘inflammation of the tendon’.
However, most tendon problems (apart from fresh tendon injury) DO NOT involve inflammation. So both the terms tendonitis and tendinitis are usually incorrect.
In some rheumatological conditions, the tendon and tendon sheath can be inflammed, so the term tendinitis can be used correctly in this instance.
Is tendinitis the same as tendinopathy
These are often used interchangeably, but they are different.
As discussed, tendinitis literally means ‘inflammation of the tendon’.
Tendinopathy means broadly ‘a problem or disorder of the tendon’ and is a more correct term to describe tendon problems.
It is a better term because it doesn’t make any assumptions about the ‘pathology’ or what is going on inside the tendon. It is just a ‘problem tendon’.
In any reputable physio or medical literature, they will refer to tendinopathy, whereas in stock standard internet fare and lower quality medical information, it is often called tendinitis, tendonitis or tendinosis.
Is tendinopathy painful?
By definition tendinopathy is painful, because it is a clinical condition that describes pain and altered function of the tendon.
This is independent of any pathology in the tendon, meaning that you can have tendinopathy with or without changes in the tendon on imaging.
Degenerative change in the structure of the tendon, independent of clinical symptoms, is called tendinosis.
The relationship between tendon changes and pain is an interesting one.
Many diagnostic ultrasound studies show that you can have tendinopathy-type changes of a tendon without having pain. This can be quite challenging to understand, but it demonstrates the poor correlation of imaging results and pain.
This is just one study that illustrates this point with runners.

The basics of tendons
In simple terms, tendons connect muscles to bones. They transfer the force that a muscle creates onto a bone, which then creates movement at a joint. They have an internal design that makes them ideal for transmitting large forces.
Tendons act like springs to make your movement more efficient. During tasks like running, your Achilles tendon is able to store and release energy. This allows you to run further with less energy.
Everywhere there is a muscle, there is a tendon. Usually there will be at least one tendon from a muscle and sometimes two. The region in which the muscle becomes tendon is called the musculotendinous junction.
Tendon composition
Tendons are collections of tightly-bound collagen fibers that are surrounded by small amounts of water and tendon cells, tenocytes and immature tendon cells, tenoblasts.
This is all contained within a tendon sheath that holds everything in place.
Tendon tissue is a great example of another way in which the human body is capable of adaptation. It can adapt by becoming stronger and more resilient if it is given the right amount challenge.
Tendon tissue is another example of ‘use it or lose it’ in the human body.
Conversely, tendon tissue can adapt by becoming less resilient and less tolerant of work if it isn’t used as much.
It is the tenocyctes that respond to challenge. When a mechanical load is placed on the tendon, tenocytes respond by creating more collagen and other tendon components.
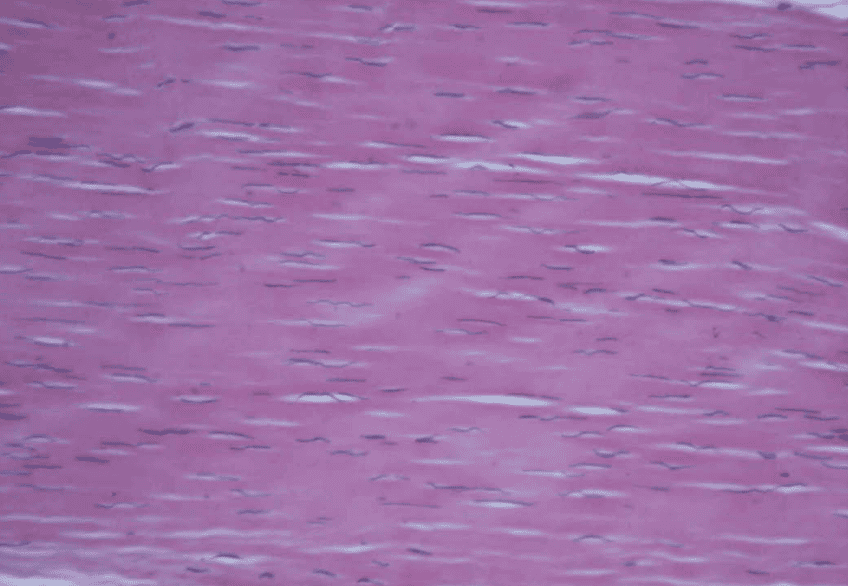
As you can see in this image of healthy tendon, the collagen fibres are aligned in one direction so that they can transmit force efficiently.
The dark elongated structures are the nuclei of the fibroblasts known as the tenocytes, which manufacture the collagen and other substances of the tendon.
Tendon properties
Tendons don’t have the ability to create their own force by shortening like muscle does.
However, they are able to store elastic energy and return that energy with recoil.
As tendons are mostly collagen, they don’t change length as the muscle contracts.
This means that as the muscle contracts and shortens, the force is efficiently transferred from the tendon onto the bone, leading to movement.
This site has a more indepth account of tendon anatomy that is still approachable to read.
Tendon load
There are different ways that the load on a tendon is increased:
- Time eg doing the same activity but over a longer time
- Weight eg doing the same activity but with while carrying extra weight
- Intensity eg doing a similar activity but faster. For example jjumping puts more load through an Achilles tendon than doing a calf raise. The higher you jump, the more load
Any of these individually or in combination can create overload.
What happens in tendinopathy?
Current evidence suggests that tendon pathology is different to the pathology seen in most other tissues. The experts recognise that what happens in the tendon isn’t fully understood, but there is agreement on these aspects.
A tendinopathy is essentially a load intolerance problem, meaning that it is caused by excess loads that are above the tendon’s usual capacity.
Though not the only cause of tendinopathy, this is the most frequent cause for the condition.
When this happens, the tendon can’t keep up with the demand that is being placed on it. As a result, it has injury, tries to heal and fails to do so adequately.
The most popular explanation is that overload makes the tendon cells (tenocytes, tenoblasts) become activated and proliferate. These cells produce more of some of the tendon components that have the effect of mucking up the collagen arrangement which makes the tendon less capable of coping with load. More blood vessels grow into the tendon tissue, and more nerve fibres do as well.
It is often labelled a ‘failed healing response’.
Tendinopathy can affect the mid-portion of the tendon or the attachment point of the tendon onto the bone, called insertional tendinopathy or enthesopathy.
These two areas have nuances that mean that treatment needs to be different.
Apart from the tendon tissue itself, there are other structures of the tendon that can become a problem. The layer that encloses the tendon can become painful too, and this can be called tenosynovitis or peritendinitis.
The treatment strategies for each of these are quite different.
The common causes of tendon pain
Overload causing tendon pain
The most common cause of tendon pain is overuse or overload.
This occurs when there is an increase in load or activity that the tendon doesn’t have the time or capacity to adapt to.
These sudden changes in activity can happen over days to weeks.
An example of a tendinopathy occuring over days is a weekend of gardening. It can lead to issues like ‘tennis elbow’ (elbow pain that is often from tendinopathy of the common extensor tendon) where there is a sudden increase in gripping activities such as grabbing, lifting and digging.
Unless you work as a landscaper and your tissues are used to the load, or you gradually increase gardening over weeks and months, this sudden burst of activity leads to cumulative load on the tendon over the weekend.
Conversely, overuse injuries sometimes take a few weeks to appear.
Chronic overload is when a higher load is maintained over longer periods of time, like 3-4 weeks. The load is not enough to not prompt an acute response but with the load being increased each week, eventually tendon pain starts.
The main risk factors for an overloading a tendon are:
Taking up a new exercise or activity e.g. starting running for exercise, a sudden burst of gardening
Changing intensity or type of exercise eg changing from strength training to high intensity training like F45
Increasing volume of exercise eg increasing running distance training for a marathon or increased repetitive movements like pruning at particular times of the seasons
Tendons require a certain period of time to adapt to a change in activity. The length of time and tolerance to change is different for everyone.
Otherwise the tendon ends up trying to adapt and change structurally but just can’t keep up with requirements.
Injury to tendons
Tendon injury can be caused by a direct blow to the tendon.
Tendons are designed to transfer force in the line of the tendon. The alignment of the tendon fibres demonstrate this function.
Tendons don’t tolerate compressive forces well, particularly from a direct blow.
This kind of injury usually leads to the start of a tendinopathy. It needs to be treated like a tendinopathy that has occurred due to overuse.
Underlying medical conditions
There are other risk factors that can be involved in tendon pain apart from injury or overload.
There are underlying medical conditions or particular life stages that increase the risk of developing tendinopathy or tendinitis.
Some of these medical conditions include:
Obesity,
Diabetes,
Hypertension
High Cholesterol
Low level systemic (whole body) inflammation created by these medical conditions is thought to be responsible for the higher rate of tendon problems.
Women going through menopause are also at a higher risk of developing tendon issues. This is thought to be related to the effect of hormonal changes.
Tendons can be involved in the inflammatory process of some inflammatory diseases like rheumatoid arthritis.
Would you like to speak with one of our physios FREE OF CHARGE?
What’s holding you back? Let’s talk about it!
BOOK ONLINE or call us on (08) 7282 0871 and let’s lock in a time!
NB: This offer is for Adelaide residents only.
How to tell if you have tendinopathy
Like any problem, correct treatment starts with correct diagnosis.
Symptoms
The main ‘tendonitis’ or tendinopathy symptoms are pain and the sensation of tendon stiffness.
Tendinopathy has a typical behaviour pattern which can make it easier to differentiate from other problems.
In the early stages, the pain isn’t there all the time, and it is very load -dependent, meaning it will depend on the intensity or the load of the activity.
Some activities will be quite painfree. However as the demand on the tendon increases, so does the likelihood and the intensity of pain.
Warming up phenomenon
One important feature that differentiates tendon pain from other problems is a “warming up” phenomenon, which is also known as ‘start up pain’.
This is when the main symptoms of pain and stiffness in the affected area at the start of activity, which then seems to reduce pain completely during the activity. The tendon seems to ‘warm up’.
Once the activity stops, either the pain comes back or stops for an extended period of time.
After a period of rest, the starting up pain happens and it has to warm up again.
Later stages
In later stages of tendon issues the pain in the affected area becomes more constant.
The pain is still load-dependent meaning it will still increase with activity.
However the pain doesn’t stop during or after activity, it just reduces to a dull ache as long as the activity doesn’t overload the tendon.
Signs
There will be pain if the tendon is loaded adequately. This is done by testing the muscle group that the tendon is attached to.
For example, the Achilles tendon will be painful if the calf muscle is working.
An important note is that the tendon needs to be tested adequately.
If it is in the early stages, a simple calf raise might not be enough. It might need to be repeated many times, or under more load by carrying extra weight, or doing something more dynamic like hopping.
Other signs that we would expect to find in a tendonitis (tendinopathy) are;
muscle weakness
pain on certain movements that put increase load through the tendon and
tenderness at the affected area
swelling around the tendon, appearing like a thick tendon
Diagnosis
The diagnosis of tendinopathy is made through findings from the subjective examination and physical exam.
The behaviour, the site of pain and the pain that is reproduced on loading are usually enough to make a diagnosis.
Imaging like ultrasound imaging usually isn’t helpful in diagnosing tendinopathy.
That might sound counterintuitive, but there is a high rate of tendinopathy changes in the tendons of people with no pain.

Different tendinopathy locations
Tendon pain can happen in a variety of locations in the upper body and the lower body.
Here is a list of common tendinopathies in the upper extremity:
Elbow
Tennis elbow (sometimes mistakenly called lateral epicondylitis): is a common complaint, with pain on the outer side of the elbow at the common extensor tendon. This can affect people of all ages
Golfer’s elbow (also mistakenly called medial epicondylitis): less common, affects the inner side of the elbow at the common flexor origin
Shoulder
Rotator cuff: any of the tendons of the four cuff muscles can be affected, but supraspinatus is the most commonly affected. Ultrasound often shows tendinopathic changes in people with or without pain
Long head of biceps: this is situated at the front of the shoulder
The lower limb has more sites that can be affected:
The groin muscles (hip adductors) and hamstring muscle groups can develop tendinopathy. A common cause of buttock pain is proximal hamstring tendinopathy.
These problems particularly affect people who take part in sports that involve kicking or sprinting.
Adductor and hamstring tendinopathy are featured in our article on the top 10 soccer injuries.
Gluteal tendinopathy is a common condition, in particular gluteus medius tendinopathy.
This is often misdiagnosed as ‘trochanteric bursitis’ and while there may be a thickened bursa on ultrasound, it is the failed healing response of the tendon that is usually the problem.
Gluteal tendiopathies can affect people of all ages and activity levels, but are particularly common in middle aged females.
At the knee, patellar tendinopathy at the front of the knee is a common source of tendon pain, which can be called ‘jumper’s knee’.
As the name suggests, this is common in people who engage in jumping and also running.
The Achilles tendon is a very common site for tendinitis and tendon pain. Achilles tendinopathy is common in runners and field sports. Tibialis posterior is another tendon at the ankle that is quite common to develop tendinitis or ‘tendonitis’.
Plantar fasciitis can be considered to be a tendinopathy as well, with the same pathology. The rehabilitation principles are the same as any other tendinopathy. The lack of an inflammatory component in this condition makes the ‘itis’ incorrect. It is more accurate to call this plantar fasciosis.
Physio treatment for tendinopathy
The best non-surgical treatment options are guided by the stage of the tendinopathy and the severity of pain.
Rest
Rest is commonly prescribed as treatment for tendinopathies.
Rest or some kind of reduction in activity may be helpful in the early stages of a tendinopathy. This is only as a short term option to assist with pain management.
The best rest is often not complete rest, but ‘activity modification’ to reduce excessive load temporarily. This is most effective in the early stages of tendinopathy. In some cases two weeks of rest is more than enough to stop a tendinopathy developing further.
Long-term rest may appear to fix the problem and solve the pain. Usually when the affected tendon is loaded again, the pain will reappear.
This is because there hasn’t been any rehabilitation. The tendon hasn’t been exposed to any load, and this is what stimulates it to change.
In fact it is exactly the opposite! It has been given less load and therefore it will adapt to that instead.
In summary, rest is not a good treatment strategy for an established tendinopathy.
This is where specific exercise and load is vital!
Ice
Much like rest, cold therapy is most effective in the early stages of tendinopathy.
You can consider ice to be symptomatic relief, and it is OK to use it with this in mind.
More recently there is a suggestion that there is an inflammatory process in some early tendinopathies, so a few days of ice might be helpful in managing the pain.
In the chronic tendinopathy, there is a lot of research to confirm that there is not an inflammatory response, so ice is not going to help inflammation in these tendons. But if it feels good, there is no harm in using it.
Exercise
Exercise is the most important of treatment for any tendinopathy – we can’t stress this enough!
The principle is to give the tendon some stimulus – a reason to change.
The key is providing the right exercise with the right load at the right dosage.
The right load is going to change too. As the tendon adapts, it will require more work to challenge it. This is where some assistance from a physio is key. They will be able to identify how hard you should be working and prescribe the exercises and the dosage according to how you are.
Too little load won’t bring about the change you are looking for, and you are risking further injury.
Too much runs the risk of working the tendon beyond its capabilities and it not quite being able to catch up.
You are aiming for a ‘sweet zone’ – enough stimulus to drive change, but without overloading it.
Sometimes it is referred to as the Goldilocks principle: ‘not to little stress, not too much stress, just right’
This healthy amount of load is different for everyone. It depends on the person’s current activity level, their general health, age, genetics, and current tendon health.
Shockwave Therapy
Shockwave therapy is delivered by a shockwave machine which produces high frequency sound waves via an applicator head to the tendon.
This is done over a number of sessions, with an increase in the intensity of treatment from one session to the next.
The research is mixed on the success of shockwave treatment.
It is important to understand that shockwave therapy can be quite useful for pain relief.
However they do nothing for the muscle strength or the ability of the tendon to cope with load.
There may be pain relief initially, but there is a good chance that pain will recur.

Medical treatments for tendon Pain
There are a number of other strategies that can be used for tendon treatment, but the results of research is mixed.
Injections
Corticosteroid injections can be helpful for pain relief. There needs to be exercise rehabilitation started during the period of pain reduction. If not, there is a high chance that the pain will return to pre-injection levels when the cortisone wears off.
Additionally, research has shown that cortisone is cytotoxic, meaning that it can be harmful to tendon cells. Because of this, there is a limit to the number of cortisone injections that can be placed into the same tendon before it becomes harmful for the health of the tendon.
Platelet-rich plasma (PRP) injections are re-injecting the patient’s own platelets into the tendon. Platelets are an important part of the body’s healing process and the theory is that injecting a higher concentration of them they will help heal the tendon.
Despite this, the research suggests that improvement between individuals is variable. They can also be quite expensive.
Surgery
Surgery should remain the last option for managing tendinopathy. It usually consists of debriding (cleaning out) the degenerative tissue from the tendon and surrounding tendon tissue.
It is recommended that the patients are carefully selected and only after an adequate loading program has been trialled for at least a year.
Challenges of tendinopathy
Recovering from a long term tendon injury can be quite challenging. Here are a few to consider:
- The tendon with tendinopathy can be very particular about the activity that it can perform
- Doing too little won’t help – you can’t rest your way out of a tendon problem
- Overloading it certainly won’t help – you can’t push on through a tendon problem
- The time that is required at each stage can be agonisingly slow if you are dying to get back to sport, but you can’t rush it and risk overload
- The target amount of load is constantly changing, so the ‘sweet zone’ is constantly changing too.
- Other things will impact the healing process, like the immune system, the endocrine system, nervous system, general health, nutrition
- The amount of degenerative tissue in the tendon will affect its potential for full recovery.
As you can see there are many factors to consider when coming up with the right dosage and the right plan. Guidance from a physio is important to stay on track with dosage and motivation, and to make sure that the transition back to sport or function is done at the right speed.
Preventing tendon problems
There are two major things to consider to avoid tendon problems:
Tip #1: Avoid large increases in activity
Overload can be over a short period (acute) of time or over a consistent period of time (chronic).
Acute overload usually occur when starting a new exercise routine or starting pre-season training for sport.
-
To avoid overuse, change need to be made slowly and incrementally
-
Rest days must be included in your program
-
Maintain fitness in the off-season from sport to avoid problems in the pre-season period
Chronic overload is when a higher load is maintained over a longer period of time, usually 3-4 weeks or more. Often the load is manageable in the early stages and does not prompt an acute response but as the load is increased each week the signs and symptoms of tendinopathy begin.
To avoid chronic overload, a deloading week should be considered, where activity is maintained but the load is reduced. This allows the tendon to maintain its strength without being overloaded.
Tip #2: Maintain strength exercises
Tendons do require physical demand to maintain their health. They are another ‘use it or lose it’ example like muscle, bone, cardiovascular fitness and much more.
Your level of activity will determine how often strength training is required.
During pre-season for sport, strength training should be maintained 2-3 time per week but reduced to once a week during season.
With activity like running, strength training should be maintained at 1-2 times per week.
Would you like to speak with one of our physios FREE OF CHARGE?
What’s holding you back? Let’s talk about it!
BOOK ONLINE or call us on (08) 7282 0871 and let’s lock in a time!
NB: This offer is for Adelaide residents only.
Common questions about tendons and tendinopathy
What is the best way to treat a tendonitis?
The answer is going to depend on the stage of the tendonitis (tendinopathy). For example, if it is tendon pain that has only just occured after being overloaded, then relative rest and ice will be helpful. However, the longer the tendonitis has been present, the less likely this strategy is going to solve the problem. In that case, a graduated loading program is going to be the best form of rehabilitation. This needs guidance from a trained physiotherapist to get the dosage right from the beginning.
Will tendonitis go away on its own?
If the ‘watch and wait’ approach is taken, usually the result will be it will settle down until the tendon is challenged again, at which time you can expect the tendonitis to become a problem again.
What is the main cause of tendonitis?
There are some health conditions that make tendons more susceptible to tendonitis. Most of the time, tendonitis happens as the result of overloading the tendon by using the tendon more than it is conditioned.
How long does it take for tendonitis to heal?
The symptoms of an acute ‘reactive’ tendonitis may settle relatively quickly ie within days. The more longstanding the tendon problem, the longer that you can expect it to take. A loading program needs to be over a period of time that allows the tendon to adapt, so it doesn’t happen as quickly. You might be looking at anywhere between 6 to 12 weeks or longer for a tendon to regain its capacity without pain.
What can I do to help my tendinopathy to heal quicker?
When it comes time to help the tendon to adapt its structure, that is a different situation!
Hopefully you’ll understand after reading this article that it takes graduated load and challenge for the tenocytes to provide adaptation to the tendon structure. This is by far the most important thing that you can do to help accelerate the process of reducing pain and increasing your function.
Is tendinopathy the same as arthritis?
These are very different conditions with different underlying problems. Arthritis is often thought of as a joint cartilage problem (though it is much more than that!). Tendinopathy is something that affects tendon tissue only. The symptoms and behaviour of these problems are quite different.
Summary
- Tendons are an essential component of our body that allows us to move and perform everyday activities
- Overload, overuse injury, and underlying medical conditions are common causes of tendon pain
- It is essential to understand the signs and symptoms of tendinopathy
- There are various types of tendinopathies that can occur throughout the body, which can lead to significant discomfort and pain
- By understanding the basics of tendons and the concepts tendinopathy, you can take steps to avoid it, or if it occurs, to manage and prevent it from affecting your daily life
Other articles that might be of interest:
Ankle sprains – A comprehensive look at a common injury, but an injury not well managed.
Soccer injuries – An interesting breakdown of the 10 most common soccer injuries and why they happen.
Jumper’s knee – Kimberley Wilson has written this blog on a condition that is very common amongst volleyballers, basketballers and kangaroos















