If you have neck and headache pain and you type the question ‘can your neck cause headaches?’ into a search engine, the answer is ‘this is called cervicogenic headache’.
Unfortunately, that is where it stops.
While there is no doubt that the cervical spine can produce headaches, we also know that the category known as cervicogenic headache is just scratching the surface.
The experience of physios and patients tells us that this is a gross underestimation of how entwined the cervical spine is with headache problems.
This article is worth reading if you:
- are getting treatment for your neck because you feel like it is the cause
- have been told that your neck is the problem by a health professional but you aren’t really sure
- have been told your neck isn’t the problem, but you aren’t convinced?
- haven’t had any treatment to your neck but you instinctively feel like it might be involved in some way
At the end of this, you’ll know:
- the traditional way of thinking about the neck and head pain problems
- the way that your neck is potentially related to all head pain
- the types of head pain that can have cervical spine involvement, including headache and migraine types
- how to find out if your neck is involved with your head pain
There is also a really easy clue to confirm that your neck is involved.
Let’s get started!
The Traditional Thinking Regarding the Neck and Head Pain
In the traditional medical model, the neck is only involved with cervicogenic headaches or ‘neck-based headaches’.
In this model, the neck has no role to play in any other headache type, and certainly doesn’t have a role to play in migraine.
However, the neuroanatomical basis for possible cervical spine involvement in all head and face pain is easy to understand. It has been established and accepted for decades.
However the body of research to support the involvement of the cervical spine in headache types hasn’t been strong. This has resulted in the International Headache Society estimating that cervicogenic headache is rare.
To rate even cervicogenic headache as ‘rare’ would come as a surprise to every physio, chiro, osteopath and headache sufferer.
Most of the research that has been conducted into the role of the cervical spine and head pain has concentrated on cervicogenic headache.
But this only scratches the surface …
The Important Piece Of Neuroanatomy You Must Understand
There is an expanding body of evidence that sheds light on what happens with headache and migraine sufferers.
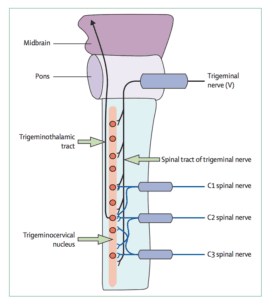
A key bit of neuroanatomy is the trigeminocervical nucleus in the lower brainstem.
We have created a consumer-friendly review of the trigeminocervical nucleus and how it is involved in producing head pain.
You can see a research article written by two of the pre-eminent migraine researchers here.
The trigeminocervical nucleus receives information from two main areas: the head and face, and also from the upper three segments of the neck.
It has been shown to become extra-sensitive in headache and migraine sufferers.
Not only that, it has been found to remain sensitised in between bouts and not just during the episode of headache or migraine.
This means that it is primed and takes less to ‘tip it over the edge’.
An event that ‘tips it over the edge’ can be any number of things.
This could be smell, food, alcohol, hormonal change during menstrual cycle, an increase in muscle tension or a prolonged posture.
So The Neck Could Be Involved In Any Kind Of Head Pain?
Yes.
Any sensory information transmitted by the spinal nerves of the upper neck has the ability to sensitise the trigeminocervical nucleus.
This could be the result of a ‘grumpy’ joint, muscle, disc or any of the structures that are services by these levels of nerves.
This means that any altered function of the upper three segments of the neck is capable of sensitising the trigeminocervical nucleus.
5 Simple Exercises For Headache Relief
Need some simple neck exercises to help with headaches?
This article presents our top 5 exercises plus one stretch that everyone gets shown (but we NEVER use).
Types Of Head Pain That Can Be Influenced By The Cervical Spine
A wide range of head pain problems can have a neck component influencing them:
- cervicogenic headache (neck headache)
- tension-type headache
- migraine of all types
- silent migraine
- cluster headache
- SUNCT
- trigeminal neuralgia
- sinus pain
Does Neck Pain Mean That Your Neck Is The Cause Of Your Headache?
The answer is ‘no’.
Pain can be felt in the neck as part of a migraine aura, or during the course of a headache without being the reason behind the headache or migraine.
Neck pain can be a referred phenomenon as opposed to the root cause.
The trigeminocervical complex means that neck pain is a common feature of migraine and headache, in the same way that the upper neck can contribute to the head pain that is experienced.
However, this is the argument that is used to say that neck pain is never the cause.
How Can You Find Out If Your Neck Is Causing It?
The best way is to have your problem assessed by a headache physio who is trained in the Watson Headache Approach.
They will be able to identify if there is a relevant link.
On their own, these features won’t help you know if your neck is definitely involved:
- Neck range of movement
- Neck pain
- Reproduction of head pain on palpation
- Tenderness of neck muscles
- Headache or migraine that starts in the neck or shoulders
All of these features may be present in a problem that has its origins in your neck, but they aren’t definitive on their own.
For example, it is possible to reproduce head pain in a lot of people by palpating certain joints in the neck.
Unfortunately, the neck is often blamed or ruled out by professionals who don’t have the skills to perform a systematic examination.

Is There An Easy Way To Tell?
There is one really simple feature that tells you that your neck is very likely to be involved, and it isn’t neck pain, tenderness or loss of movement.
Through many years of observation and treatment of headache and migraine sufferers, Dr Dean Watson has discovered this feature.
If your headaches or migraines swap sides ever, your neck is the number one culprit until proven otherwise.
So what exactly does that mean?
It might be that your headaches are on one side mostly and only occasionally happen on the other side
It might be that your head pain starts on one side. Then swaps to the other side within the same episode (and sometimes back again).
This doesn’t mean that if your head pain is only ever on one side (‘sidelocked’), or if your head pain is completely symmetrical, that your neck isn’t involved.
However, it means that if headache and migraine conditions show any swapping behaviour, your neck definitely deserves to be considered.
Do You Need To Have Neck Pain?
The answer is NO!
Often if someone doesn’t get neck pain, they dismiss their neck as a possible cause for a headache and migraine condition.
For example, a lot of people suffer from headache and migraine conditions that seem to have a relationship to their menstrual cycle, and they dismiss their neck as a possible cause.
This isn’t the case at all – you don’t need to have neck pain for your neck to be an important cause.
Summary
Despite the general dismissal of the role of the neck in headache conditions, it isn’t hard to understand the theoretical basis for it.
In practice, the rate of success in treating headaches of all types, including migraine, underpins this.
If you have head pain, headache or migraine and you aren’t satisfied with your situation, your management or your diagnosis, you deserve to have assessment of your upper cervical spine to either rule it in or rule it out.
This assessment can be done by a physio trained in the Watson Headache Approach.













